HUMAN
REPRODUCTIVE SYSTEM
1. Male reproductive system
It consists
of Paired testes, Accessory ducts,
Accessory glands and external genitalia.
-
Testes are
formed within the abdomen. Soon after the birth or at the 8th month
of pregnancy they descent into the scrotal
sac (scrotum) through inguinal canal.
-
The low
temperature (2-2.50 C less than the body temperature) of scrotum
helps for proper functioning of testes and for spermatogenesis.
-
Each testis is oval in shape. Length 4-5 cm, width: 2-3 cm.
-
Each testis has
about 250 testicular lobules. Each lobule contains 1-3 coiled seminiferous tubules.
-
Seminiferous
tubule is lined internally with spermatogenic
cells (spermatogonia or male germ cells) & Sertoli cells (supporting cells).
-
Sertoli cells
give shape and nourishment to developing spermatogenic cells.
-
The regions
outside the seminiferous tubules (interstitial spaces) contain
· Small blood vessels.
· Interstitial
cells or Leydig cells. They
secrete testicular hormones (androgens).
· Immunologically competent cells.
b. Accessory
ducts (Duct system)
- Include rete testis, vasa efferentia, epididymis & vas
deferens.
- Seminiferous tubules unite
to form straight tubules → open into rete testis (irregular
cavities) → Vasa efferentia (series of fine tubules that conduct sperms) → epididymis (stores
sperms temporarily) → vas deferens → join with a duct from seminal vesicle to form common ejaculatory duct → opens into urethra → urethral meatus (external opening).
-
The urethra receives
the ducts of prostate and Cowper’s glands and passes through the penis.
c. Accessory glands
-
Include a prostate gland, a pair of seminal vesicles
and a pair of Cowper’s glands
(bulbo-urethral glands).
-
Their collective
secretion (seminal plasma) is
rich in fructose, Ca and enzymes.
It
· Helps for transporting sperms
· Supplies nutrients to sperms
· Provides an alkaline medium to counteract the acidity of the
uterus.
· Secretions of Cowper’s
glands lubricate the penis.
d. Penis (external genitalia)
-
It is a copulatory organ made up of special erectile
spongy tissues which when filled
with blood causes the erection. It facilitates insemination.
-
The cone-shaped
tip of the penis is called glans penis
which is covered by prepuce (foreskin).
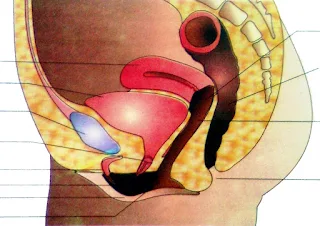
2. Female reproductive system
It includes Ovaries, Accessory ducts & External genitalia.
- Primary sex organs which produce ova
(female gamete) & steroid ovarian
hormones (estrogen &
progesterone).
-
Ovaries are
located on both side of the lower abdomen.
-
Each ovary is
about 2-4 cm in length and is connected to the pelvic wall and uterus by
ligaments.
-
Each ovary is
covered by a thin epithelium which encloses the ovarian stroma.
-
The stroma has
outer cortex and inner medulla.
-
Ovary contains groups
of cells (Ovarian or Graafian follicles).
Each follicle carries a centrally placed ovum.
b. Accessory ducts (Duct system)
-
Include 2 oviducts (Fallopian tubes), a uterus &
vagina.
-
Each oviduct (10-12 cm long) has 3 parts such as
· Infundibulum: Funnel-shaped opening
provided with many finger-like fimbriae.
It helps to collect the ovum after the ovulation (release of ovum from ovary).
· Ampulla: Wider part.
· Isthmus: Narrow part. It joins the uterus.
-
The ciliated epithelium lined the lumen of
the oviduct drives the ovum towards the uterus.
-
Uterus (womb) is
inverted pear shaped.
-
It is supported by ligaments attached to the pelvic wall.
-
Uterus has 3
parts- Upper fundus, middle body and terminal cervix. Cervix opens to vagina.
-
Vagina opens to the exterior between urethra
and anus.
-
The uterine
wall has 3 layers such as
· External perimetrium (thin membrane)
· Middle myometrium (thick layer of smooth muscle)
· Inner glandular and vascular endometrium.
-
The lumen of
vagina is lined by a glycogen-rich mucous membrane consisting of sensitive papillae and Bartholin’s glands. The secretions of
Bartholin’s glands lubricate the penis during sexual act.
-
Consist of Mons pubis, vestibule, hymen &
clitoris.
- Mons pubis: A cushion of fatty tissue covered by pubic
hair.
-
Vestibule: A median channel. It includes
· Labia majora: Large,
fleshy, fatty and hairy outer folds. Surrounds vaginal opening.
· Labia minora: Small,
thin and hairless inner folds.
-
Hymen (Maiden head): A membrane which partially
cover the vaginal opening. It is often torn during the first coitus. It can
also be broken by a sudden fall or jolt, insertion of a vaginal tampon; active
participation in some sports items etc. In some women, hymen persists even
after coitus. So the hymen is not a reliable indicator of virginity.
-
Clitoris: A highly sensitive organ lying just in front of the urethral
opening.
-
Glandular
tissue of each breast has 15-20 mammary lobes containing clusters of
cells (alveoli).
-
The cells of
alveoli secrete milk which is stored in the cavities (lumen) of alveoli.
-
The alveoli
open into mammary tubules.
-
The tubules of
each lobe join to form a mammary duct.
-
Several mammary
ducts join to form a wider mammary ampulla which is connected to lactiferous
duct through which milk is sucked out.
GAMETOGENESIS
-
It is the formation
of gametes in the gonads.
- Includes Spermatogenesis
and Oogenesis.
-
It is the
process of formation of sperms (spermatozoa) in seminiferous tubules of testis.
It has 2 stages: Formation of spermatids
and Spermiogenesis.
a.
Formation of spermatids: In this, Spermatogonia (Sperm mother cells or immature male germ cells)
produce spermatids.
b.Spermiogenesis:
Spermatids transform into sperm.
Schematic representation of spermatogenesis
Spermatogonia -2n (Diploid, 46 chromosomes)
↓ Mitosis
differentiation
Prim. spermatocytes (2n)
↓1st meiotic division
Sec. spermatocytes -n (Haploid, 23 chromosomes)
↓2nd meiotic division
Spermatids (n)
↓ Differentiation
Spermatozoa (n)
-
Each Primary spermatocyte
produces 2 secondary spermatocytes.
Each secondary spermatocyte produces 2 haploid
spermatids. Thus 4 spermatids
are formed from each primary spermatocyte.
- After
spermiogenesis, sperm heads become embedded in the Sertoli cells and are
finally released from seminiferous tubules. It is called spermiation.
Role of Hormones in Spermatogenesis
-
Hypothalamus
releases large amount of Gonadotropin releasing hormone (GnRH).
-
GnRH stimulates
the anterior pituitary gland to secrete 2 gonadotropins such as Luteinizing
hormone (LH) & follicle stimulating hormone (FSH).
-
LH acts on the Leydig
cells and stimulates secretion of androgens. Androgens stimulate the
spermatogenesis.
- FSH acts on the
Sertoli cells and stimulates secretion of some factors which help in the
process of spermiogenesis.
-
A mature sperm
measures about 60 µ (0.06 mm) long.
-
A plasma
membrane envelops the whole body of sperm. Sperm consists of
a.
Head: Oval shaped. Formed of nucleus
and acrosome. Acrosome is formed
from Golgi complex. It contains lytic enzymes. Behind the head is a
neck containing proximal and distal centrioles.
b.
Middle piece: Composed of axial filament surrounded by mitochondria
and cytoplasm. Mitochondria produce
energy for the sperm motility.
c.
Tail: Consists of a central axial
filament. The sperm moves in fluid medium and female genital tract by the undulating movement of the tail.
-
Sperms are transported by the accessory ducts. Secretions of epididymis,
vas deferens, seminal vesicle and prostate are essential for maturation and
motility of sperms.
-
Seminal plasma & sperms together constitute the semen.
-
The human male ejaculates about 200-300 million sperms during a coitus.
- For normal fertility
at least 60% sperms must have normal shape and size. 40% of them must show
vigorous motility.
2. Oogenesis
-
It is the
process of formation and maturation of ovum.
-
It takes place
in Graafian follicles.
- Oogenesis is initiated in embryonic stage when
millions of egg mother cells (oogonia) are formed within each ovary.
-
No more oogonia
are formed and added after birth.
- Oogonia multiply to form primary oocytes. They
enter into prophase-I of the meiosis and get temporarily arrested at
that stage.
-
Each primary
oocyte gets surrounded by a layer of granulosa cells to form primary
follicle.
-
A large number
of primary follicles degenerate during the phase from birth to puberty. Therefore
at puberty only 60,000-80,000 primary follicles are left in each ovary.
- Primary follicles get surrounded by more
layers of granulosa cells and a new theca to form secondary
follicles.
-
The secondary
follicles transform into a tertiary follicle. It has a fluid filled
cavity (antrum). The theca layer forms an inner theca interna and
an outer theca externa.
-
The primary
oocyte within the tertiary follicle grows in size and undergoes first unequal meiotic
division to form a large haploid secondary oocyte and a tiny first
polar body. The secondary oocyte retains the nutrient rich cytoplasm of the
primary oocyte.
-
It is unknown
that whether the first polar body divides further or degenerates.
-
The tertiary
follicle further changes into the mature follicle (Graafian follicle).
-
Secondary oocyte forms a new membrane (zona pellucida).
- Graafian
follicle now ruptures to release the secondary oocyte (ovum) from the
ovary. This is called ovulation.
Schematic
representation of oogenesis

Oogonia (egg mother cells)-2n (46
chromosomes)
↓ Mitosis differentiation
Primary
oocyte- 2n (grow in size)
↓ 1st meiotic division (prior
to ovulation)
Secondary
oocyte (n) & first polar body (n)
↓ 2nd meiotic division (during
fertilization)
Ovum (n)
& second Polar body (n)
Comparison between Spermatogenesis & Oogenesis
Spermatogenesis
|
Oogenesis
|
·
Occurs in
testis
|
Occurs in ovary
|
·
Limited
growth phase
|
Elaborated growth phase
|
·
Each primary spermatocyte
gives 4 sperms
|
Each primary oocyte gives only one
ovum. Polar bodies are formed.
|
·
It begins at
puberty and extends up to senility
|
It begins at embryonic stage and
suspended at the time of birth. The remaining part takes place only after
puberty.
|
-
Spherical and non-motile. About 0.2 mm in diameter.
-
Ovum has 4
membranes:
a.
Plasma membrane (Oolemma): Innermost
layer.
b.
Vitelline membrane: Attached to plasma membrane.
c.
Zona pellucida: Transparent
non-cellular layer found outer to the Vitelline membrane.
d.
Corona radiata: Outer layer
formed of follicle cells. These
cells are found together by hyaluronic
acid.
MENSTRUAL CYCLE (REPRODUCTIVE CYCLE)
-
It is the
cyclic events starting from one
menstruation till the next that take place during the reproductive period (from puberty to
menopause) of a woman’s life. Its duration is 28 or 29 days.
-
Menstrual cycle is also seen in other primates.
Menstrual
cycle includes
a. Ovarian cycle: Changes in ovary.
b. Uterine cycle: Changes
in uterus, oviduct and vagina.
Menstrual
cycle has the following phases
I. Menstrual phase: 1-5th day
-
The cycle starts with menstrual flow (bleeding).
-
It lasts for 3-5 days.
-
It is due to breakdown of endometrial lining and blood vessels of the
uterus that comes out through vagina.
-
Menstruation occurs if the released ovum is not fertilized.
-
Lack of menstruation may be indicative of pregnancy.
It may also be caused due to stress, poor
health etc.
II. Follicular
(Proliferative) phase: 5-13th day
-
It starts from 5th day after menstruation
and completed within 8-12 days.
-
In this phase, the action of gonadotropins (FSH
&LH) from pituitary occurs. FSH stimulates
o
Development of primary follicles into Graafian follicles.
o Secretion of oestrogens by Graafian follicles.
-
Oestrogens
stimulate
o Proliferation of ruptured
uterine endometrium and mucous lining of oviduct & vagina.
o Development of secondary sexual characters.
o Suppression of FSH secretion.
o Secretion of LH
(Luteinizing hormone).
III. Ovulatory
phase: 14th day
-
LH & FSH
attain a peak level in the middle of cycle.
-
Rapid secretion
of LH (LH surge) induces rupture of Graafian follicle and thereby ovulation
(on 14th day).
IV. Secretory (Luteal)
phase: 15-28th day
-
After ovulation,
Graafian follicle is transformed into a yellow endocrine mass called Corpus luteum. It secretes progesterone. By the action of
progesterone,
o
Endometrium attains maximum
vascularity, thickness and softness.
Thus the uterus gets ready for implantation.
o FSH secretion is inhibited to prevent development of a second
ovarian follicle.
-
During
pregnancy all events of menstrual cycle stop and there is no menstruation.
-
If fertilization
does not occur, corpus luteum degenerates and becomes a whitish mass (corpus albicans). As it has no secretory ability, progesterone level
in blood decreases. It leads to menstruation
indicating a new cycle.
§ Menarche: The
first menstruation during puberty.
§ Menopause: Stopping
of menstrual cycle (at about 50 yrs of
age).
FERTILIZATION AND IMPLANTATION
-
During
copulation, semen is released by the penis into the vagina (insemination).
Sperms → vagina → cervical canal → uterus → isthmus
↓
Fertilization
← Ampullary-isthmic Junction
↑
↑
Ovum (from ovary) → fimbriae → infundibulum
→ ampulla
-
Fertilization (sperm + ovum → zygote) occurs
only if ovum & sperms are transported simultaneously. So all copulations do
not lead to fertilization & pregnancy.
-
A sperm contacts
with zona pellucida. It induces changes in the membrane that block entry
of additional sperms.
-
With the help of secretions of the acrosome, sperm enter into the
cytoplasm of the ovum. This causes second meiotic division of the secondary
oocyte to form a second polar body and a haploid ovum (ootid).
-
The haploid
nuclei of the sperm and ovum fuse together to form a diploid zygote.
- Sex determination (See chapter 3).
-
The mitotic
division (cleavage) starts as the zygote moves through the isthmus
towards the uterus and forms 2, 4, 8, 16 daughter cells called blastomeres.
-
The embryo with
8-16 blastomeres is called a morula.
- Morula continues to divide and transforms into
blastocyst.
-
The blastomeres
in the blastocyst are arranged into an outer layer (trophoblast) and an
inner group of cells (inner cell mass) attached to trophoblast.
- The trophoblast layer then gets attached to
endometrium and the inner cell mass gets differentiated to 3 germ layers (outer
ectoderm, middle mesoderm & inner endoderm). This 3-layered structure (gastrula)
forms the embryo.
- After attachment, uterine cells divide rapidly
and cover the blastocyst. As a result, the blastocyst becomes embedded in the
endometrium. This is called implantation.
PREGNANCY AND EMBRYONIC DEVELOPMENT
-
After implantation, finger-like projections (chorionic villi) appear on the trophoblast which is surrounded by the uterine tissue and
maternal blood.
-
The chorionic villi & uterine tissue become interdigitated with each
other and form placenta. It is a structural and functional unit b/w embryo (foetus)
and maternal body.
-
Placenta is connected to the embryo by an umbilical cord. It transports
substances to and from the embryo.
-
Functions of placenta:
· Acts as barrier between the foetus and mother.
· Soluble
inorganic and organic materials, nutrients, hormones, antibodies, etc can
pass through the placenta from the mother to foetus.
· Helps in the gas exchange
between mother and foetus.
· Elimination of nitrogenous
wastes of foetus.
· Acts as an endocrine gland by secreting Human chorionic gonadotropin (hCG), human
placental lactogen (hPL), oestrogens, progesterone and relaxin.
-
During
pregnancy, levels of estrogens, progestogens, cortisol, prolactin, thyroxine
etc are also increased in maternal blood. They support the fetal growth,
metabolic changes in the mother and maintain pregnancy.
-
The germ layers
give rise to all tissues (organs). The stem cells in inner cell mass have
the potency to give rise to all the tissues and organs.
-
Human pregnancy
(gestation period) lasts 9 months (for cats: 2 months, dogs: 2 months,
elephants: 21 months).
Changes in embryo during pregnancy:
- After one month of pregnancy: Heart is formed.
End of second month: Limbs and digits are developed.
End of 12 weeks (first trimester): The major organs (limbs, external genital organs etc)
are well developed.
During 5th month: First movement
of foetus and appearance of hair on the head.
End of 24 weeks (second trimester):
Body is covered with fine hair, eyelids separate and eye lashes are formed.
End of 9 months: Ready for
delivery.
PARTURITION AND LACTATION
-
Parturition (labour): Process of giving birth to young ones.
-
Parturition is
induced by neuroendocrine mechanism.
-
The signals originating from the foetus and placenta induce mild uterine
contractions (fetal ejection reflex). This causes the release of oxytocin
from maternal pituitary.
-
Oxytocin causes
stronger uterine muscle contractions which in turn stimulate further secretion
of oxytocin. This process is continued leading to expulsion of the baby out of
the uterus through the birth canal.
-
After parturition,
the umbilical cord is cut off.
-
The placenta &
remnants of umbilical cord are expelled from the maternal body after
parturition. It is called “after birth”.
-
The mammary glands produce milk towards the end of pregnancy by the
process called lactation.
-
The yellowish milk produced during the initial
few days of lactation is called colostrum. It contains several antibodies essential to
develop resistance for the new born babies.